Ehlers-Danlos Syndrome (EDS) is a rare, inherited group of disorders that affect the connective tissues in the body. These tissues, which include skin, joints, blood vessels, and internal organs, provide structure and support to the body. EDS is caused by a genetic mutation that affects the production of collagen, a protein that plays a critical role in the strength and elasticity of connective tissues. The condition leads to a wide range of symptoms, varying in severity, and can significantly impact an individual’s quality of life. This article aims to explore the causes, types, symptoms, diagnosis, treatment options, and living with Ehlers-Danlos Syndrome.
What is Ehlers-Danlos Syndrome?
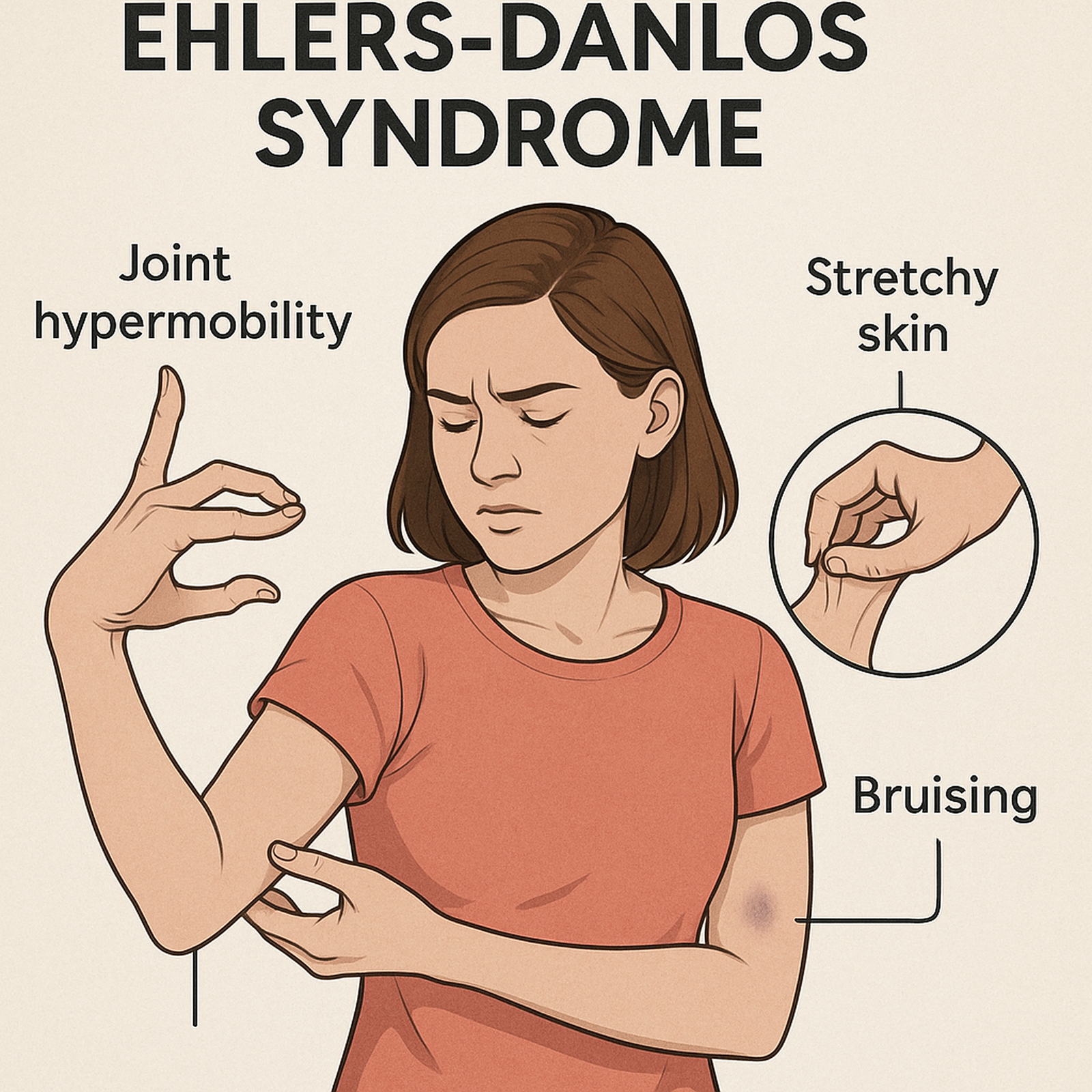
Ehlers-Danlos Syndrome is a group of genetic disorders that affect the body’s connective tissues. The connective tissue provides structure, strength, and elasticity to the skin, joints, blood vessels, and organs. Individuals with EDS have defects in collagen, the protein that makes connective tissues strong and flexible. As a result, people with EDS may experience a range of symptoms, including hyperelastic skin, joint hypermobility (excessive movement of the joints), and increased risk of bruising, bleeding, and scarring.
EDS is inherited in different ways, meaning it can be passed down through families. It can be caused by mutations in various genes, and depending on the mutation, the severity of symptoms and the specific type of EDS can vary greatly from one person to another.
Types of Ehlers-Danlos Syndrome
There are 13 recognized types of Ehlers-Danlos Syndrome, each with unique features and symptoms. However, the most common and well-known types include:
- Classical EDS: Characterized by hyperelastic skin, which is soft, velvety, and often fragile. People with classical EDS also experience joint hypermobility, leading to frequent joint dislocations and subluxations. Scarring may be unusual, and individuals can have a tendency to develop bruises easily.
- Hypermobility EDS (hEDS): This is one of the most common types of EDS, characterized by joint hypermobility without the severe skin involvement seen in classical EDS. People with hEDS often experience chronic pain, joint instability, and a higher risk of dislocations and injuries.
- Vascular EDS (vEDS): One of the most serious forms of EDS, vascular EDS affects blood vessels, leading to a higher risk of arterial rupture, organ rupture, and internal bleeding. People with this type of EDS are at risk for life-threatening complications due to the fragility of blood vessels.
- Kyphoscoliotic EDS (kEDS): This type is characterized by scoliosis (curvature of the spine), muscle weakness, and hypermobility. Unlike other forms of EDS, kyphoscoliotic EDS also affects the eyes and can lead to vision problems.
- Arthrochalasia EDS: This type is associated with severe joint hypermobility and frequent dislocations. People with arthrochalasia EDS may experience a loss of collagen in the skin, causing the skin to be fragile and prone to injury.
- Dermatosparaxis EDS (dEDS): People with dEDS often have extremely fragile skin that can easily tear or bruise. This type also affects the joints, which may be hypermobile. The skin tends to sag and is extremely soft.
While these are the most common types of EDS, the condition is diverse, and some individuals may have a combination of symptoms from different types. As the underlying genetic mutations are better understood, new types of EDS may be identified.
Symptoms of Ehlers-Danlos Syndrome
The symptoms of Ehlers-Danlos Syndrome can vary significantly depending on the type, but there are several common features that many individuals share:
- Hyperelastic Skin: One of the hallmark symptoms of EDS is skin that stretches more than normal. In classical types of EDS, the skin is unusually soft, smooth, and can be hyper-elastic, meaning it stretches more than typical skin. However, the skin may tear or bruise easily.
- Joint Hypermobility: Individuals with EDS typically have joints that move beyond the normal range of motion. This can lead to frequent joint dislocations, subluxations (partial dislocations), and chronic joint pain. Hypermobility can also result in muscle weakness and fatigue.
- Fragile Blood Vessels: Particularly in vascular EDS, the blood vessels, organs, and tissues are fragile and prone to tearing. This can lead to life-threatening complications such as ruptured blood vessels, internal bleeding, and organ damage.
- Chronic Pain: Many people with EDS experience chronic musculoskeletal pain due to joint instability and muscle weakness. The pain can be widespread and may worsen with age.
- Delayed Wound Healing and Scarring: People with EDS often experience poor wound healing. Scars may be wide and thin, and the skin may be prone to excessive bruising.
- Fatigue: Due to chronic pain, joint instability, and muscle weakness, many individuals with EDS experience chronic fatigue. This can be exacerbated by poor sleep, which is common among people with this condition.
- Other Symptoms: Depending on the type of EDS, individuals may experience problems with internal organs, such as gastrointestinal issues, early-onset osteoarthritis, or problems with vision, hearing, and heart function.
Diagnosis of Ehlers-Danlos Syndrome
Diagnosing Ehlers-Danlos Syndrome can be challenging, as its symptoms often overlap with other conditions. A thorough clinical evaluation by a specialist, typically a geneticist or rheumatologist, is essential for diagnosis. The process usually includes:
- Family History: Since EDS is inherited, the doctor will ask about any family history of similar symptoms.
- Physical Examination: The doctor will look for signs of hypermobility in the joints, hyperelastic skin, and other features associated with EDS.
- Genetic Testing: Genetic tests can confirm the presence of mutations in the collagen genes. This is particularly important for diagnosing rare forms of EDS.
- Biopsy: In some cases, a skin biopsy may be performed to examine the structure of collagen and confirm the diagnosis.
Treatment and Management
Currently, there is no cure for Ehlers-Danlos Syndrome, but the symptoms can be managed with appropriate treatment. Management typically focuses on reducing symptoms, improving quality of life, and preventing complications.
- Pain Management: Due to chronic joint pain, individuals with EDS may benefit from pain management strategies, including physical therapy, medications, and sometimes corticosteroid injections.
- Physical Therapy: Physical therapy is critical for strengthening muscles and improving joint stability. This can help reduce the risk of joint dislocations and prevent further damage to the joints.
- Surgical Considerations: Surgery should be approached with caution, as people with EDS may experience complications such as poor wound healing, scarring, and bleeding. If surgery is necessary, it is important to consult with a specialist familiar with EDS.
- Lifestyle Adjustments: To reduce the risk of injury, individuals with EDS are advised to avoid activities that put excessive strain on the joints and connective tissues. Supportive devices like braces or splints may be recommended to stabilize the joints.
- Regular Monitoring: People with vascular EDS require regular monitoring of their cardiovascular health due to the increased risk of arterial rupture and other vascular issues. Regular check-ups are important for managing potential complications.
Living with Ehlers-Danlos Syndrome
Living with Ehlers-Danlos Syndrome can be challenging, as it requires careful management of symptoms and potential complications. Psychological support, such as counseling or joining support groups, can be invaluable in helping individuals cope with the emotional and mental health challenges that come with a chronic condition.
In addition to medical treatment, lifestyle changes like practicing gentle exercises, wearing protective gear, and avoiding activities that could cause injury are crucial for managing daily life with EDS.
Conclusion
Ehlers-Danlos Syndrome is a complex genetic disorder that affects the body’s connective tissues, leading to a wide array of symptoms, including hyperelastic skin, joint hypermobility, and fragile blood vessels. While there is no cure for EDS, a combination of medical treatments, physical therapy, and lifestyle adjustments can help manage the condition. Early diagnosis, proper care, and ongoing management are essential for individuals with EDS to live fulfilling lives despite the challenges posed by the condition.